January 22 -- 25 Weeks, 5 Days
We had our first visit at Mott Children's Hospital in Ann Arbor. Blaine's parents came Wednesday night so they could stay with Carsyn while we were gone at our appointments. That night I woke up at 3:45AM. I don't know why it was such a big deal, but I was so worried because I had forgotten to change Carsyn's poopy diaper before bed. I think I was so worried because I was also so anxious for our appointments. I could't fall back asleep, so I got out of bed around 5:15 to get dressed. Once Blaine woke up and we were just about to walk out the door, I said I felt bad because I forgot to change Carsyn's diaper before she went to sleep so she's been sleeping in a poopy diaper all night. Blaine said he changed her before he put her in bed. Well shucks, all that worry for no reason!
Every single doctors appointment really puts me on edge. I do get worried of the bad news that could be said, as the past few appointments have snowballed with bad news after bad news. We arrived to Mott's a bit early, but it gave us a few minutes to find Blaine some coffee and find our way to our first appointment. There we had a full body ultrasound in fetal diagnostics. Blaine and I were both amazed with how nice all the equipment was. We have seen plenty of ultrasounds, and the pictures we were seeing was almost in ultra high definition. Once the tech was done, the maternal and fetal medicine doctor came in to talk with us about what she saw. She said she wanted to take a closer look at some things that she wasn't seeing clearly, oh great, here we go again. She began looking closely at Kennedy's lips and nose looking for deformations, then to her ears. She said everything was looking good, and she turned the picture to 3D. There she was, the most beautiful little girl I have ever seen, along with her big sister. It nearly brought tears to my eyes, and it really made my heartache. How can something so "perfect" be going through so much. I was so happy to see that face, nose, ears, and fingers. So perfect, so little. It brought me a sense of hope. Once we were done with the doctor, we met with a genetic counselor, which was very laid back. We then headed up to the 11th floor where the pediatric cardiac floor was located. Up next, a fetal echo. Blaine and I were both getting heavy eyes, and having the fetal echo done in a dark room wasn't helping at all. The bed I was laying on was so comfortable, and laying there watching the flutter of Kennedy's little heart on the screen was really making my eyes even more heavy. The cardiologist came in to take a look at some things for herself, then we sat down and discussed the next steps.
She confirmed the findings that Kennedy does in fact have an intact atrial septum. We have two choices: 1). Fetal Intervention or 2.) Surgery immediately when she's born. With both come many risks:
Fetal Intervention:
- There is a 10% chance she would not survive after intervention.
- I could go into preterm labor, and if she is premature, there would be almost no chance of saving her.
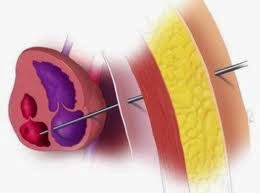
- There are a few other complications that could happen, as they would be sticking a needle into a blood filled organ (her heart), and anything the needle would go through (my belly, the amniotic sac, her chest, and her heart), there is a possibility of bleeding and not being able to stop it.
- As there are risks with any type of surgery, the risks to me are much less than the risks to her.
Immediate Surgery After Delivery
- There is a 50% chance she would not survive, as babies with intact septums are born very sick and go downhill very quickly.
- They would deliver her via C-Section (probably in the cath lab) then move her across the room and operate immediately as they would have to for any chance of survival.
- Since these babies come out very sick, there is a chance she wouldn't be strong or big enough to make it through the first surgery.
As fetal intervention is still very new and very rare, it's still in an experimental stage. They aren't sure if there are any long term benefits to doing fetal intervention, but they believe that by doing so it prevents 8-10 weeks of damage to the lung vessels. If we do decide to go with the intervention, after delivery they would monitor her until they feel they are ready to operate. In the first surgery, they will look at her aorta and decide if it is capable of doing its job. If her aorta is big enough, she will have a pulmonary band placed on her pulmonary artery to regulate blood flow to the lungs. If her aorta is too small, she will have to have the Norwood procedure done. The Norwood is a higher risk surgery, as it is a bypass. Once they determine her aorta's status and give her the proper surgery, she will still be receiving the next two surgeries: Hemi-Fontan (Glenn) around 3 months and the Fontan between 18 months and 3 years. The cardiologist did say that both procedures have been successful, but ultimately we have to do what we feel is best for us.
Both scenarios absolutely terrify us. It's still hard to come to terms with the fact that I could lose my little girl. Blaine and I both feel as though we aren't quite ready to make a decision yet, but something is telling us to do intervention. I would do anything to give her one more chance to fight, anything. I pray God will take my hand and lead me to what is best for her. I already feel like He has pulled me in that direction, because it's not the "facts" or statistics that make me feel like this is best. It's the feeling in my heart and gut that this is what I must do. The cardiologist said they will be aiming to do intervention around February 24 (30 weeks). They still have to coordinate with all the doctors and make sure everyone is available and can be there on that day. We will plan and schedule the date for the intervention and begin the insurance pre-approval process. We will continue to pray and let God help us through this and make sure this is the best decision, and pray the insurance will cover as much of the surgery expense as possible, as this is one more major medical expense we will have to pay for a large chunk of that we weren't planning on. As hard as it is to try and not stress about money, which has not been easy for months since I haven't been able to find a job, this has really put the cherry on top. Money IS a big deal when it comes to the possible expenses we will have to face, and it is a reality we have to consider.
I am sure you all are wondering what the intervention process would be like for us. The surgery is an outpatient surgery. I would get an epidural, and they would just give me one dose and wouldn't keep administering more because they may need me to get up and move around to get her in the perfect position she needs to be in. Once she is there, they will give me more epidural, and give her a shot in the arm, butt, or leg (whichever is the easiest access to give her anesthesia, a sedative type drug to prevent her from moving, and something else to help with her healing). The doctors will place a large needle through my belly, through her chest cavity, and directly into her heart. They will blow up a tiny balloon connected to a wire through the needle, and place a shunt in the septum wall to keep it open. The doctors would monitor her for a few minutes and make sure blood is flowing through the hole (which they say can be seen immediately). The whole process is done using sonogram. The incision site on me would be so little there would only be one or two stitches, unless they use glue, and it's so little it can fit under a bandaid. From there, they continue to monitor her to make sure she isn't bleeding into the paracardial sac, or have any other complications. They would let my epidural wear off and once I can do all the things the epidural disrupts, I am free to go home. I would have to return to Ann Arbor within the next few days for them to check her again to make sure she is doing ok. I wouldn't be placed on bedrest or anything extreme for recovery, they recommend to take it easy for a few days following. Since every appointment is scheduled by the hospital, we don't really get to pick our days, and with the surgery we have to do it when all the doctors are open. Of course, the week they plan to do it is the week of indoor Big Tens in Cleveland. Blaine will probably have to leave that Wednesday, and won't be back until late Saturday. I am so thankful for the staff he works with and under and that they are allowing him to go to all of our appointments. I don't think I could go to them on my own or with anyone else and be ok. I pray we can have intervention the week before or that Tuesday they are planning on before he would have to leave. It's already so hard on him to have to leave at all, especially at such an important time.
 |
| Kennedy 25 Weeks |
 |
| Fetal Cardiac Intervention |
 |
| Fetal Cardiac Intervention |
 |
| Fetal Cardiac Intervention |
 |
| Fetal Cardiac Intervention |
I haven't been sleeping very well the past couple nights since our appointment at Mott's. I can't stop seeing her little face, and I think about her so often. I've felt so tired, but I can't get a good sleep. I can feel myself tossing and turning the whole night I am sleeping. This weekend I have kept myself decently busy. I had to work a MSU hockey game last night (Friday), one today, and I have a MSU women's basketball game tomorrow. Blake came and visited today, and watched Carsyn for us while Blaine was at Notre Dame for a meet and when I had to leave for the game. We've always managed to do everything with Carsyn on our own. I've only had people watch her a handful of times (all of which I can count on one hand, we may have hit two hands today and the majority when we are home for a few hours). Besides that, I've always taken her everywhere. I wish we could live closer to Blake. He has been one of my best friends since I have known Blaine. He probably knows a lot more about me than most brother-in-laws should know about their sister-in-law, but he's really been a saving grace in my life. Carsyn loves him so much. She used to cry just seeing him a few months back, so I am so happy she gets excited to see him. It's been an overwhelming week. As a new month is upon us, I keep thinking of everything that awaits us beginning February 1.
I want to thank everyone for keeping our family in their thoughts and prayers. Every prayer for our sweet Kennedy is special and we thank you so much. Please keep sharing our page and our fundraiser. "Every little bit makes a difference." I have had a few people reach out to me about our situation, one of those people has really made an impact in my life, and I am glad I can do the same for her. Please say a prayer for her as her little girl needs them desperately also.
 |
| Kennedy 25 Weeks |
God Bless You All,






